PPG Info Page - Community Health and Care
LBMP area Community Health and Care Services - updated January 2023
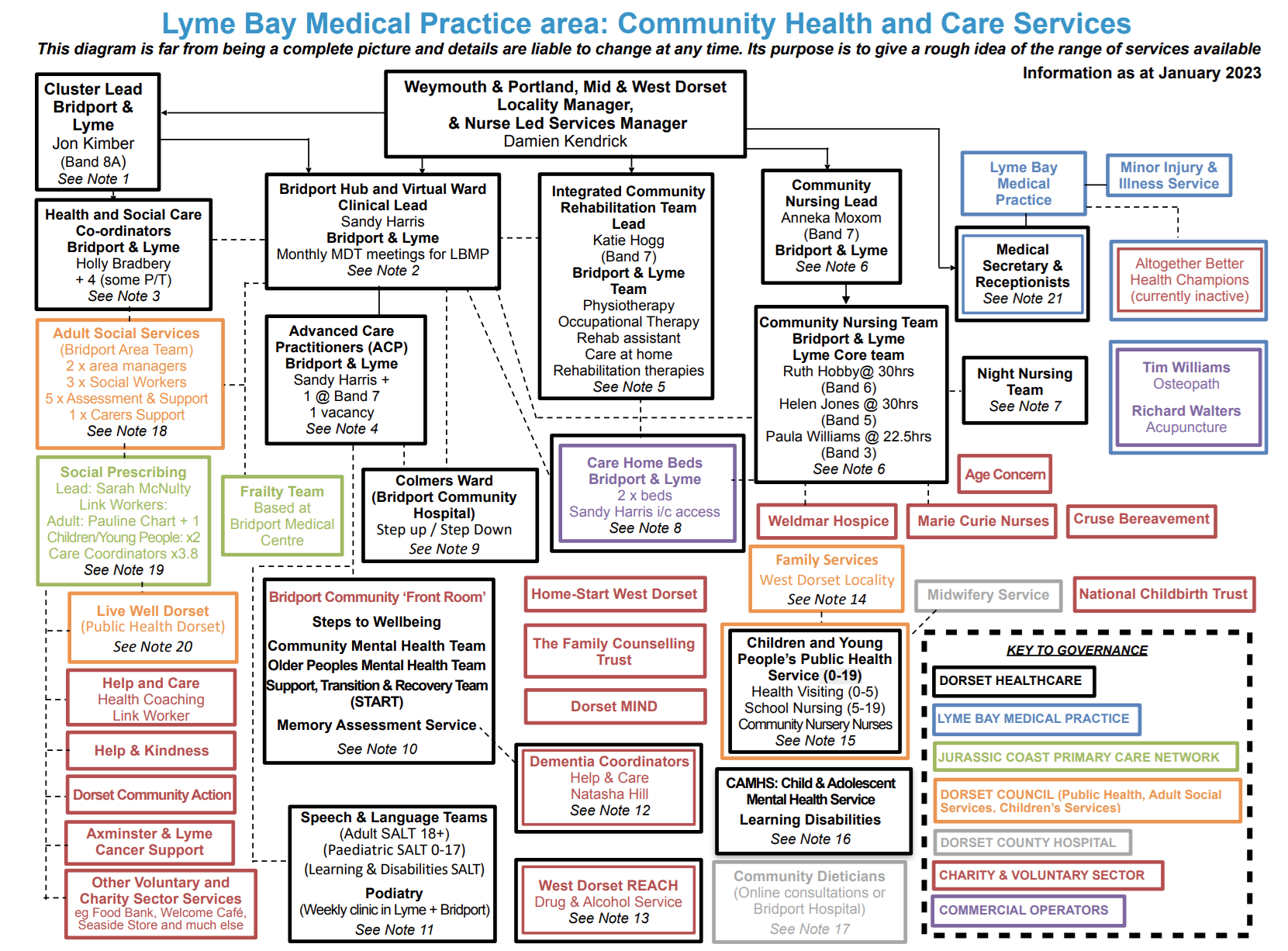
The diagram below is far from being a complete picture of the Community Health and Care Services in the Lyme Bay Medical Practice area. Details are liable to change at any time. Its purpose is to give a rough idea of the range of services available.
This information may be downloaded and viewed as a PDF document by following this link>>
Notes on the Diagram (as at January 2023)
- John Kimber leads the ‘Single Point of Access’ that links General Practice, Community Nursing and Rehabilitation, acute hospitals (especially discharge home or care with support) and Social Services. He leads the four-times-daily Zoom-based virtual meetings of his team to identify needs and coordinate appropriate patient care, linking to the work of the ‘Virtual Ward’ and the Bridport Hub, based at Bridport Community Hospital.
- The ‘Hub’ is a central clearing house which brings together the full range of professionals, both health and social services, concerned with the care and treatment of patients.The aim of the Hub, in drawing together the various services, is to prevent unnecessary hospital admissions and to manage care after discharge where hospital is unavoidable. The ‘Virtual Ward’ monitors patients being cared for at home, coordinating services provided by community nursing and rehabilitation teams. Sandy Harris leads a monthly Zoom-based virtual Multidisciplinary Team Meeting (MDT) to review LBMP patients identified as needing ongoing care. The notes about MDT meetings (page 4) show the typical composition and working method for these meetings, and for the input to the Hub.
- The Health and Social Care Coordinators work across NHS and Social Services boundaries to arrange coordinated provision of services.
- The Advanced Care Practitioners oversee the medical aspects for the Virtual Ward, community nursing and rehabilitation services.
- The Integrated Community Rehabilitation Team covers Bridport and LBMP areas, working flexibly according to need. There are no specifically LBMP-related staff. Occupational therapists help people to resume or maintain participation in their jobs, leisure and social activities, getting around, caring for themselves and their home, etc.
- The Community Nursing Team provides all aspects of nursing care to the housebound, including continence assessment & advice and wound care, working closely with GPs and patient carers. Community nurses also provide palliative care, working with Marie Curie nurses and Weldmar Hospice. The team covers Bridport and LBMP areas, used flexibly according to need. The three named nurses are generally dedicated to working in the LBMP area and are based at the Medical Centre for most of their time. The nursing team works 8.00am to 8.00pm. Combining Bridport and LBMP areas for the Community Nursing and ICRT teams offers a greater range of expertise and professional support as well as improved flexibility.
- Night nursing operates from 8.00pm to 8.00am, 7 days a week, with a registered nurse and a health care assistant travelling as a pair with essential nursing equipment available. The service is Dorset-wide.
- Provision of two NHS beds in an appropriate Nursing Home is still out for tender as a two-year contract, funded by Dorset HealthCare. Sandy Harris will act as ‘gatekeeper’ for admissions and discharges. When the contract is completed, money saved from the reduction in beds from its previous level will be reinvested in extending the Community Nursing / ICRT provision for the LBMP area.
- Bridport Community Hospital has one ward of 24 beds. Admission and discharge are coordinated via the ‘Single Point of Access’ and the Hub.
- There is a lot more to mental health provision. Those listed have most direct relevance to local patients. ‘Steps to Wellbeing’ holds face-to-face counselling sessions for Lyme Bay Medical Practice patients at Kent House, as well as at home (online or by telephone). Mindfulness courses are currently online only. The service accepts self-referrals.
- The Podiatry Service runs clinics in Lyme on Tuesdays (morning, afternoon or all day depending on the type of clinic), or patients can be seen at Bridport. Referral by clinical professionals only.
- The Dementia Coordinator service is managed by the charity Help & Care under contract to Dorset HealthCare. At least one coordinator works in each Primary Care locality, providing personal support to each patient diagnosed with dementia. The coordinator for the LBMP area is Natasha Hill.
- West Dorset REACH provides advice & information for drug and/or alcohol users aged 18 and over. or those concerned about someone’s use, including prevention and recovery services and needle exchange. Based in Weymouth, it runs a Recovery session at the Bethany Chapel in Lyme on Mondays from 12.00-1.30. Self-referral or referral by health / care professionals. Partner agency EDAS provides services for under-18s.
- The West Dorset Locality of Family Services (formerly the West Family Partnership Zone) is part of the County Council’s Social Services provision for children and families. It is based at Bridport Children’s Centre. The team identifies children, families and carers in need of help, and supports them with training courses and family visits.
- The service includes health visiting, maternal support, and the national childhood measurement programme. The LBMP area is served by the West Dorset Locality Health Visiting Team (0-5) based at Bridport Medical Centre, covering also the Bridport, Maiden Newton and Beaminster areas. The Health Visiting team consists of 6 Health Visitors and a Public Health Staff Nurse, plus two Community Nursery Nurses. Toni Green is the Health Visitor working mainly with families in Lyme Regis and Charmouth. For School Nursing (5-19) every school in Dorset has a named school nurse who maintains regular contact with their school to promote healthy lifestyles and offer practical advice, information and support. The team has links with other health professionals including community paediatricians, health visitors, GPs and speech and language therapists. For Woodroffe this is Jo Mckernan (School Nurse/Team Coordinator) covering for Kerry Burrows who is on a 3 month sabbatical. St Michael’s, Charmouth, Marshwood and Thorncombe primary schools are covered by School Health Nursery Nurses and a Public Health Staff Nurse responsible to the Team Coordinator. School-age immunisation is handled separately by the Dorset School Aged Immunisation Service.
- The Child and Adolescent Mental Health Service provides support to children and young people who are coping with significant mental health difficulties, and their families and carers. The Community Learning Disability Team comprises specialist nurses, psychologists, psychiatrists, physiotherapists, occupational therapists, social workers and speech and language therapists to offer practical help with physical and mental health problems, relationships, behaviours and communication, as well as advice on issues such as finance, employment and housing.
- The Community Dietician Service is provided by Dorset County Hospital, holding consultations either ‘virtually’ or at Bridport Hospital.
- Adult Social Services (West Locality) is based in Bridport, with two parallel teams also covering the LBMP area. These teams together comprise two team managers, three social workers and seven Assessment & Support Coordinators. A Carers Case Worker covers the whole Dorchester and West Dorset Locality.
- The Social Prescribing team gives an all-age service providing personal support in improving health and wellbeing, navigating the health and care systems, advocacy as necessary, and linking to appropriate services in the voluntary sector. Self-referral or referral by health / care professionals.
- LiveWell Dorset provides ‘tailored guidance and support to help people become more healthy’. Focus on physical activity, weight loss, smoking and drinking (less!). Free ‘wellness’ advice and 20 minute 1:1 telephone ‘health coaching’. Signposting to other services. Self-referral or referral by health / care professionals.
- At the merger of Lyme Regis Medical Centre and LBMP in June 2019, employment of administration staff became the responsibility of Dorset HealthCare (as did the management of the building and grounds). More recent appointments to the administration team have been to direct employment with LBMP.
A note on the Primary Care Network.
PCNs are intended to improve collaboration between GP Practices and to bring economies of scale, a more diverse ‘skill mix’ into general practice, a greater range of services, and easier integration with the wider health and care system.
The Jurassic Coast PCN comprises the Ammonite Health Partnership (Bridport Medical Centre, Maiden Newton and Beaminster Tunnel Road), Lyme Bay Medical Practice, and Barton House in Beaminster. It is based at Bridport Medical Centre.
Advertised services are: Integrated Frailty Service, Integrated Respiratory Service, Integrated Diabetes Service, Severe Mental Illness Physical Health Checks, Clinical Pharmacy & Pharmacy Technicians, Social Prescribing, ‘group consultations’. Staff include a Dietician and a Podiatrist. See www.jurassiccoastpcn.nhs.net; this includes a useful ‘Patient Information’ section which duplicates, though with somewhat different format and content, similar information on, for example, the LBMP and Dorset HealthCare websites, among many others.
A note on Record systems.
SystmOne links GP Practices, Dorset HealthCare and some Hospitals: within each patient’s records are, where applicable, care plans relating to their specific need. (SystmOnline as used by patients within the GP Practice is separate.) RIO is the system used for mental health services; MOSAIC is used for Adult Social Services.
Health and Social Care Coordinators at the Bridport Hub can access SystmOne, RIO and Mosaic. (The Dorset Care Record is a different matter and still a ‘work in progress’).
NOTES ON MULTI-DISCIPLINARY TEAM MEETINGS (as at January 2023)
(These notes are distilled almost verbatim from 31 pages of NHS Dorset guidance, so do not necessarily apply in all respects to either LBMP or the Bridport ‘Hub’ …)
The purpose of the MDT meeting is:
- To provide a multi-disciplinary forum for the discussion and management of relevant patients
- To discuss a manageable list of identified patients who would benefit from MDT discussion or more detailed review & assessment
- To ensure that the patient is at the centre of the MDT decision making process
- To ensure that the discussion around each patient covers all relevant points
- To maintain communication between all organisations making up the multi-disciplinary team in order to promote best practice and to ensure timely, holistic individualised care
- To agree a plan of action based on intended outcomes for the patient
MDT meetings are recommended to be run monthly with an identified list of patients from risk profiling and patients of concern put forward by clinicians.
Note: the General Medical Services contract requires Practices to routinely identify moderate and severe frailty in patients aged 65 years and over.
Attendance:
- GPs
- Nurse Practitioners
- Community matrons
- District nurses
- Health & Social Care Coordinators
- Palliative care nurses
- ICRT members – physiotherapy / OT
- CMHT – adult and older peoples
- Social Services
- Administration staff/MDT Coordinator
- Third sector representative for appropriate parts of the MDT (They should not be in attendance when discussing patients not on their caseload)
Note: All surgeries should have an MDT coordinator.
Structure of an MDT
To ensure an MDT meeting is set up to enable all team members to contribute, the following are recommended:
- The chairperson may be a clinical or non-clinical team member
- The chairperson is expected to have collated and reviewed in advance of the meeting all relevant data sources including (but not exclusively): palliative care patients, admissions data, frailty and hub reports provided by the H&SC Coordinator, and identified patients from any of the multi-disciplinary teams members • GP System access available in the meeting
- All MDT members able to view GP system and relevant records
- An up to date list of all link workers attending the MDT representing their service
- The risk profiling data should be available a week in advance of the MDT to allow adequate time to gather any background information that may be helpful to the discussion
- Each patient discussed must have a clear outcome with a named person responsible for the action
- The relevant points on the MDT meeting must be recorded
- The meeting must review previous action plans from the last MDT meeting
- MDT Coordinator to follow up actions 2 weeks after meeting
Page created: 30 March 2021